Roche 454 tracks the path of "super bacteria"
In June 2011, a female patient with pulmonary infection and dyspnea was admitted to the National Institutes of Health hospital and was quickly diagnosed with Klebsiella pneumoniae, which is resistant to multiple antibiotics. During hospitalization, the hospital used the most stringent measures to prevent nosocomial infections, including isolating patients, cleaning medical devices that patients were exposed to, and so on. During the hospital stay, no nosocomial infections were found and the patient was cured and discharged in July 2011. However, after a lapse of one month, the same drug-resistant Klebsiella pneumoniae infection occurred again. In just 5 months, a total of 17 patients were infected, 10 of whom died and 6 died of Klebsiella pneumoniae. This incident has caused close attention in the hospital. Are these new cases coming from the first case? Why is the spread of super bacteria still occurring under the most stringent epidemic control measures? Is these existing disease control measures ineffective, or are there still other channels of communication that have not yet been controlled? In the event of a real infectious diseases, the researchers used the Roche 454 sequencing machine evolution of transmission of superbugs and drug resistance mutations were tracking 1. Initially using conventional pulse electrophoresis or PCR analysis, only patients infected with the ST 258 type Klebsiella pneumoniae can be identified and cannot be further subdivided. Later, the researchers used 454 to deeply sequence the isolated bacteria in the throat, bronchoalveolar lavage, groin, and urine of the first patient, and found that the original NTUH-K2044 strain in the urine, the other parts of the strain There are 7 different mutations, in which the bronchoalveolar lavage strain and the throat site have 3 mutations, the throat contains an additional mutation, and the inguinal strain contains three different mutations. Further, the strains isolated from all infected cases were sequenced, and compared with the reference NTUH-K2044 strain, a total of 41 different mutations were found. Using these mutations, these patients were divided into three groups by cluster analysis, and the most likely route of transmission was drawn in combination with the records of hospitalizations (induction time, ward, etc.).
Pain Relief Patch for Breast
Pain Relief Patch For Breast,Pain Relief Plaster For Breast,Relief For Breast Pain,Pad Relief Patch For Breast Shandong XiJieYiTong International Trade Co.,Ltd. , https://www.xjplaster.com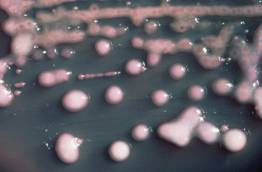
[Name] Medical Cold Patch
[Package Dimension] 10 round pieces
The pain relief patch is composed of three layers, namely, backing lining, middle gel and protective film. It is free from pharmacological, immunological or metabolic ingredients.
[Scope of Application] For cold physiotherapy, closed soft tissue only.
[Indications]
The patches give fast acting pain relief for breast hyperplasia, breast fibroids, mastitis, breast agglomera tion, swollen pain.
[How To Use a Patch]
Please follow the Schematic Diagram. One piece, one time.
The curing effect of each piece can last for 6-8 hours.
[Attention]
Do not apply the patch on the problematic skin, such as wounds, eczema, dermatitis,or in the eyes. People allergic to herbs and the pregnant are advised not to use the medication. If swelling or irritation occurs, please stop using and if any of these effects persist or worsen.notify your doctor or pharmacist promptly. Children using the patch must be supervised by adults.
[Storage Conditions]
Store below 30c in a dry place away from heat and direct sunlight.